The success rate of in vitro fertilization (IVF) is one of the most important concerns for anyone undergoing fertility treatment. It depends on multiple factors, including age, egg quality, sperm health, and medical technology. When egg quality is insufficient, choosing a high-quality egg donor can significantly increase the likelihood of success. This article explores the key factors that influence IVF outcomes and explains how to find a reliable egg donor to help you achieve your dream of becoming a parent.
Table of Contents
What Is IVF and Who Is It For?
In Vitro Fertilization (IVF) is an advanced assisted reproductive technology designed to help individuals and couples facing fertility challenges. The core concept involves combining eggs and sperm in a laboratory setting to create embryos, which are then transferred into the uterus for implantation and pregnancy.
IVF success rates are influenced by several variables, including: Age, Egg and Sperm quality, Uterine receptivity. Younger women generally have higher success rates, as egg quality declines with age, ealthy gametes are essential for viable embryo formation.
IVF success rates are influenced by several variables, including: Age, Egg and Sperm quality, Uterine receptivity. Younger women generally have higher success rates, as egg quality declines with age, ealthy gametes are essential for viable embryo formation.
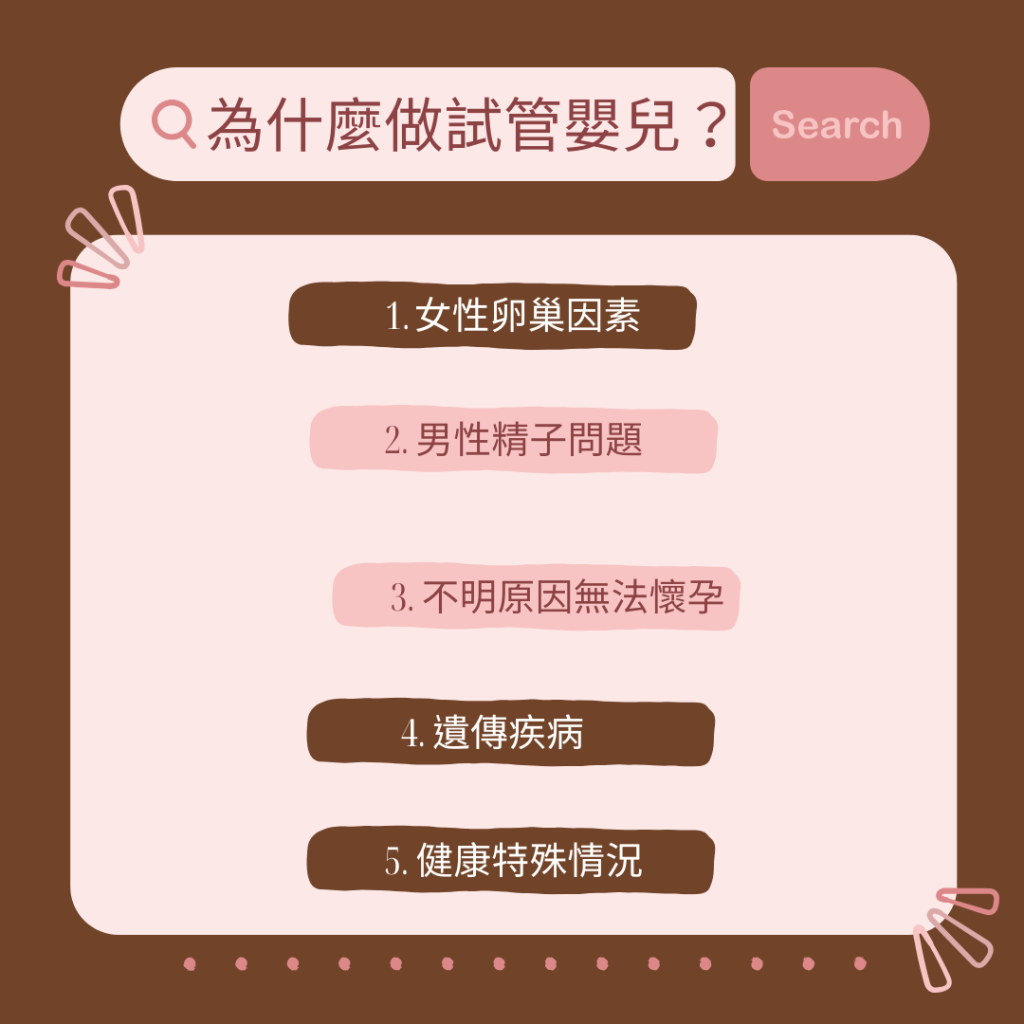
1. Female Factors Suitable for IVF
- Fallopian Tube Issues:
Blocked, damaged, or removed fallopian tubes can prevent eggs from reaching the uterus naturally. IVF bypasses the fallopian tubes entirely, making conception possible. - Ovulation Disorders:
Conditions such as Polycystic Ovary Syndrome (PCOS) or irregular ovulation can hinder egg release. IVF allows eggs to be retrieved directly after hormonal stimulation. - Endometriosis:
This condition can affect both the ovaries and uterine lining, disrupting fertilization and implantation. IVF provides an alternative path to pregnancy. - Advanced Maternal Age (35+):
As ovarian reserve and egg quality decline with age, IVF offers higher pregnancy success rates through controlled egg retrieval and embryo transfer. - Diminished Ovarian Reserve (Low AMH < 2):
Women with fewer or lower-quality eggs can benefit from IVF, which maximizes the use of available eggs or allows the use of donor eggs for higher success
2. Male Factors Suitable for IVF
- Low Sperm Count or Abnormal Sperm:
When sperm quantity, motility, or morphology is below normal, IVF combined with Intracytoplasmic Sperm Injection (ICSI) can help achieve fertilization. - Azoospermia (No Sperm in Ejaculate):
In cases where sperm is absent, it can be surgically extracted from the testes for use in IVF.
3. Unexplained Infertility
When couples have tried natural conception and other treatments such as ovulation induction or intrauterine insemination (IUI) for an extended period without success—and no clear medical cause is found—IVF is often recommended as the next step.
4. Genetic Disease Risk
Couples carrying hereditary or chromosomal abnormalities can undergo Preimplantation Genetic Testing (PGT) during IVF to ensure only genetically healthy embryos are selected for transfer.
Common examples include:
Thalassemia
G6PD deficiency (favism)
Lupus
Chromosomal translocations or deletions
PGT significantly reduces the risk of miscarriage and congenital disorders in offspring.
5. Special Health Conditions
- Cancer Patients:
Individuals undergoing chemotherapy or radiation can preserve their fertility by freezing eggs or embryos before treatment. - Using Frozen Eggs or Embryos:
Patients who have previously preserved reproductive cells for future use may choose IVF to achieve pregnancy later.
Is IVF Success Rate High?
When undergoing in vitro fertilization (IVF), choosing high-quality eggs is one of the key factors for improving success rates. With continuous advancements in reproductive medicine, we now have a deeper understanding of how egg quality affects embryo formation and implantation. High-quality eggs not only increase the likelihood of pregnancy but also reduce the risk of miscarriage.
Indicators of Egg Quality
The evaluation of egg quality mainly depends on its morphological and biological characteristics, including:
- Granulosa cell arrangement: Healthy eggs have tightly packed and evenly distributed granulosa cells.
- Cell membrane integrity: The oocyte’s membrane should appear smooth and intact.
- Nuclear status: The nucleus should be round and centrally located.
- Cytoplasmic transparency: High-quality eggs typically have clear and uniform cytoplasm.
Choosing the Right Egg Source for IVF
Whether using your own eggs or donor eggs, selecting the right source is crucial. One of the most significant factors affecting IVF success is the age and health of the eggs. Younger women generally produce higher-quality eggs. Therefore, when selecting donor eggs, it is recommended to prioritize donors who are younger, have a high number of follicles, and demonstrate a good ratio of mature eggs with excellent overall health. Choosing healthy, well-screened donors increases the chances of a successful pregnancy.
Achieving Higher IVF Success Rates
Improving IVF success is a systematic process that involves understanding egg quality indicators, selecting the right egg source, and maintaining a healthy lifestyle.
Even if the first IVF attempt is unsuccessful, cumulative success rates increase with multiple cycles — after three or more treatments, the overall success rate can exceed 60%.

How Long Does the IVF Process Take?
The in vitro fertilization (IVF) process varies depending on each individual’s physical condition and the clinic’s treatment plan. On average, a full IVF cycle takes about 1.5 to 3 months. However, including pre-treatment evaluations and psychological preparation, most patients should plan for around 3 to 6 months in total.
Below is a complete breakdown of each IVF stage and its estimated duration:
1. Pre-Treatment Evaluation and Preparation (1–2 weeks)
Couple’s Health Checkup
Includes ovarian reserve testing (e.g., AMH level), semen analysis, and hormone tests (FSH, LH, E2), along with ultrasound imaging to assess ovarian and uterine health.
Mandatory Health Tests
Both partners must submit HIV and syphilis test results from within the past six months. If not completed beforehand, these can be done during the IVF process to meet medical regulations.
Treatment Planning
Based on the examination results, the doctor tailors an individualized plan for ovulation stimulation and embryo transfer to ensure precision and efficiency throughout the IVF cycle.
2. Ovulation Induction and Monitoring (10–14 days)
- Cycle Start (Day 2–3 of Menstruation)
A baseline ultrasound is performed to count antral follicles, and hormone levels are checked via blood test. - Ovulation Stimulation
Patients take fertility medications or injections as prescribed to stimulate multiple egg follicles to mature. - Follicle Monitoring
Every 3–4 days, ultrasound and blood tests are performed to track follicle growth and adjust medication dosage. - Preparation for Egg Retrieval
When follicles are mature (around Day 14), the doctor schedules the egg retrieval procedure.
3. Egg Retrieval and Sperm Collection (1 day)
Pre-Retrieval Preparation
A trigger injection is administered 48 hours before retrieval. Patients under general anesthesia must fast for at least eight hours before the procedure.
Egg Retrieval Procedure
Mature eggs are collected transvaginally and immediately transferred to the laboratory for culture.
Sperm Collection
The male partner provides a semen sample on the same day (or a previously frozen sample may be used).
4. Embryo Culture and Selection (3–5 days)
- Fertilization
In the lab, sperm and eggs are combined to form embryos. If preimplantation genetic testing (PGT) is requested, embryos are frozen until results are available. - Embryo Quality Assessment
Healthy embryos are selected for transfer, while unused embryos are cryopreserved for future use to enhance cumulative success rates.
5. Embryo Transfer (5–10 days later)
Fresh Embryo Transfer
Embryos cultured for 3–5 days are transferred directly into the uterus. The procedure is simple and does not require anesthesia.
Frozen Embryo Transfer
For frozen embryos, 1–2 months of endometrial preparation may be needed before transfer, depending on uterine lining condition, to maximize implantation success.
6. Implantation Phase and Pregnancy Testing (≈14 days after transfer)
- Luteal Phase Support
After embryo transfer, progesterone medication is prescribed to support implantation and early pregnancy.
Pregnancy Test
About 14 days post-transfer, a blood test measures HCG levels to confirm whether pregnancy has occurred.

IVF Failure — Where to Find High-Quality Eggs?
In in vitro fertilization (IVF), choosing the right egg donor is one of the most crucial factors determining the success of the treatment.The donor’s health, genetic background, and reproductive history directly impact egg quality. Understanding these factors helps intended parents find the most suitable donor and significantly improve success rates.
1. Assessing the Donor’s Health Condition
Health status is the top priority when evaluating a potential donor. Since egg quality is closely related to overall health, each candidate must undergo thorough medical screening to ensure safety and effectiveness.
- No Genetic Disorders:
The donor should not carry hereditary diseases that could be passed on to the child. - Free from Infectious Diseases:
Screening for HIV, hepatitis B/C, and syphilis is required to avoid any infection risks during the IVF process. - Comprehensive Medical Examination:
Donors must meet medical standards through blood tests, hormone evaluations, and ultrasound scans to confirm optimal ovarian function.
Reviewing the Donor’s Reproductive History
A donor’s previous pregnancy or donation experience provides valuable insight into the potential quality of her eggs.
- Proven Fertility:
Donors who have successfully conceived or carried pregnancies often yield higher-quality eggs. - Prior Donation Success:
Previous successful egg donation cases serve as a positive indicator for both egg quality and IVF outcomes.
3. Genetic Screening and Compatibility
Genetic testing is an essential step in minimizing hereditary risks and ensuring compatibility between donor and recipient.
- Comprehensive Genetic Testing
- Ethnic and Blood Type Compatibility
Selecting the ideal donor involves both scientific evaluation and emotional alignment. The best donor should meet strict standards across medical, psychological, and genetic aspects to ensure that each egg retrieved is of high quality and suitable for embryo development.
If you’ve experienced IVF failure and want to increase your chances in the next cycle, choosing a professionally screened and medically approved donor can make a decisive difference — helping you move one step closer to your dream of parenthood.
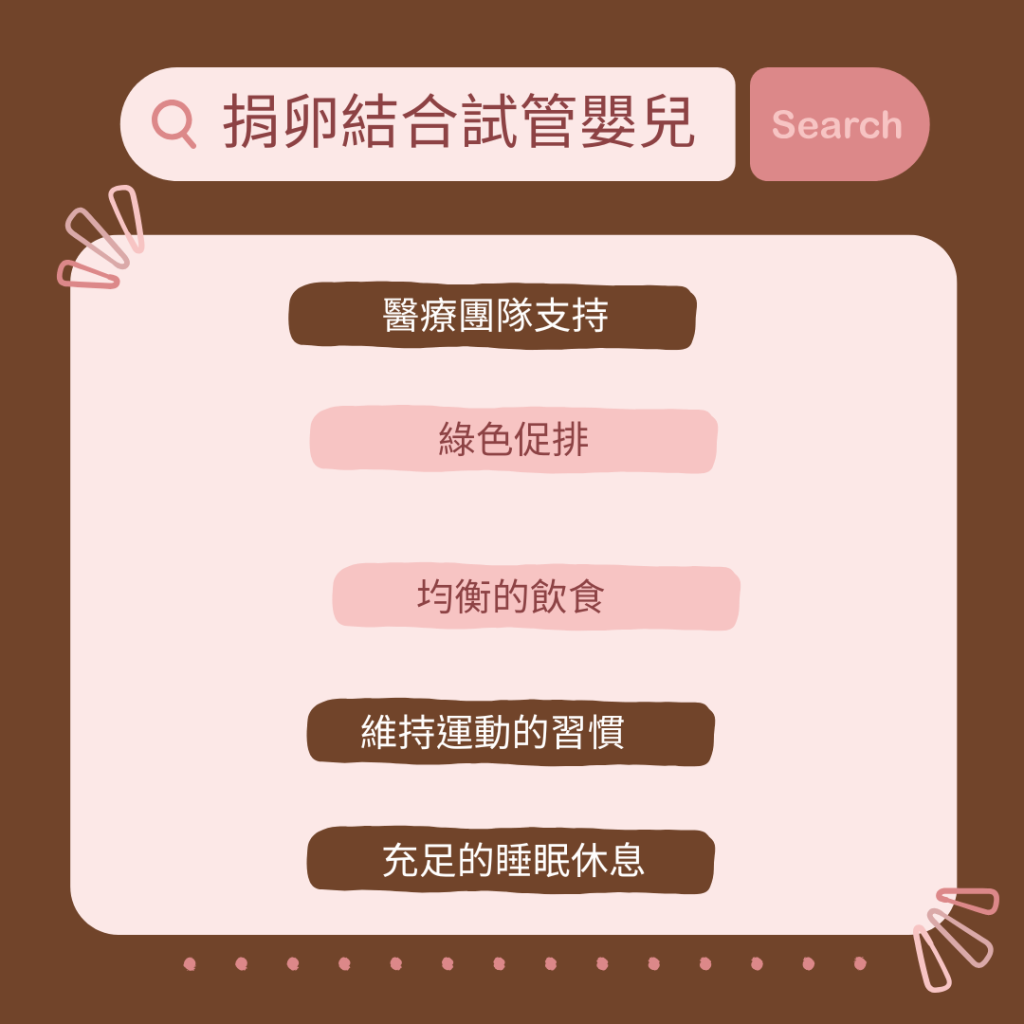
Egg Donation & IVF: Precision Fertility Treatments for Higher Success
In vitro fertilization (IVF) and egg donation bring new hope to families facing fertility challenges. IVF involves fertilizing eggs with sperm in a laboratory and then transferring the embryos into the uterus — offering a viable solution for couples struggling to conceive. When egg quality is poor, egg donation becomes a key option to boost success rates, as high-quality donor eggs combined with expert medical care can significantly increase the chances of pregnancy.
| Healthy Lifestyle & | Personalized Medical Support |
|---|---|
| Comprehensive Medical Guidance: | IVF and egg donation treatments require the support of a professional fertility team. Combining personalized treatment plans with a healthy lifestyle can greatly enhance success rates. From gentle ovarian stimulation (eco-stimulation) to precision bloodwork and immune modulation, each step plays a vital role in improving fertility outcomes. |
| Personalized Ovarian Stimulation – Eco-Stimulation | “Eco-stimulation” customizes the ovulation induction protocol based on ovarian reserve (AMH levels) and follicle count, minimizing unnecessary medication and reducing physical strain during the IVF process. |
| Balanced Nutrition | Increase intake of foods rich in vitamin D, folic acid, omega-3 fatty acids, and antioxidants, all of which support reproductive health. Avoid excessive caffeine, alcohol, and sugar, as they may affect egg quality and uterine receptivity. |
| Moderate Exercise | Engage in gentle activities such as walking, yoga, or swimming to maintain physical and emotional balance. Exercise enhances blood circulation, especially in the uterus and pelvic region, creating an optimal environment for embryo implantation. Avoid strenuous or high-impact workouts during the IVF cycle. |
| Adequate Rest & Sleep | Ensure 7–9 hours of quality sleep each night to allow hormonal balance and body recovery. Avoid staying up late or maintaining irregular sleep patterns, as these can disrupt circadian rhythms and hormone regulation. |
Common IVF Risks — What You Should Know
Common risk factors for in vitro fertilization (IVF)
Occurs when ovulation-stimulating medications cause excessive follicle growth, leading to abdominal bloating, discomfort, or fluid accumulation.
Transferring multiple embryos can increase the likelihood of twins or triplets, which raises pregnancy and delivery risks.
Rarely, issues such as implantation failure or ectopic pregnancy may occur after embryo transfer.



